Authors

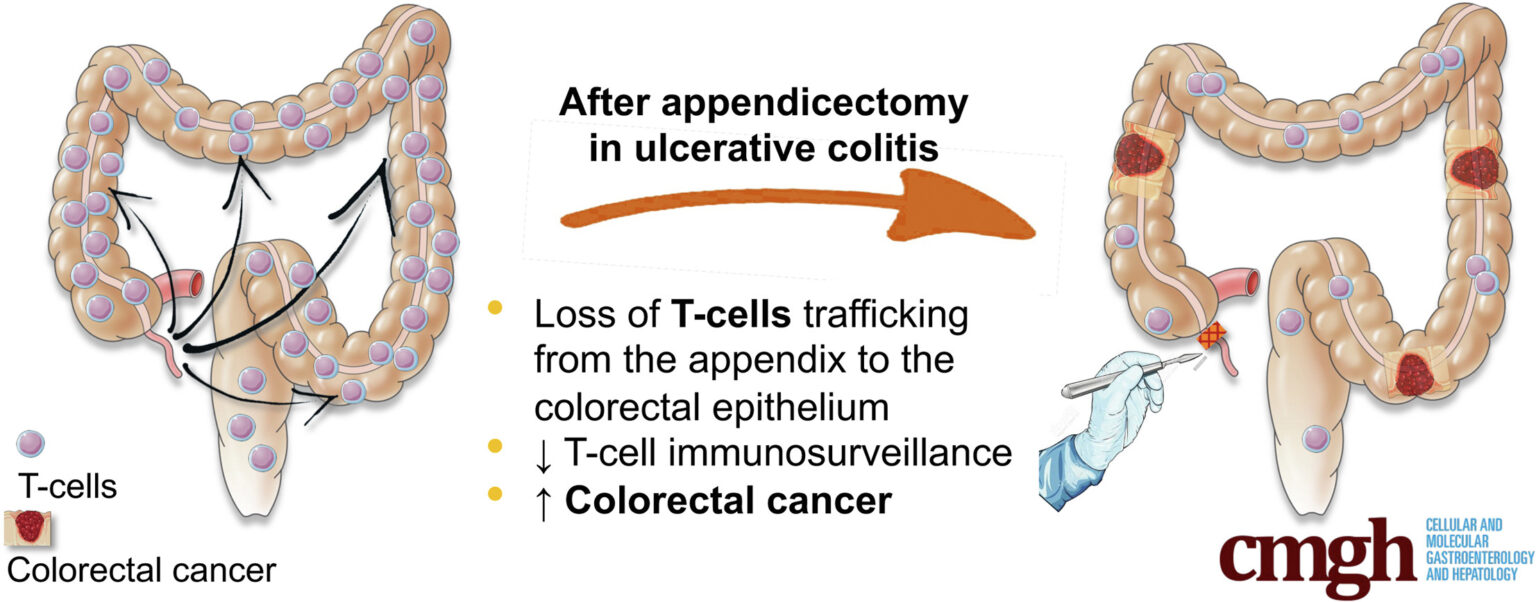
Appendectomy is known to reduce colorectal inflammation in patients with ulcerative colitis (UC). But some data have suggested that this surgical procedure is associated with an increased risk of colitis-associated cancer (CAC).
To confirm these data and understand its mechanism, mice underwent appendectomy, appendicitis or laparotomy. They were then exposed to azoxymethane/sodium dextran sulfate (AOM/DSS) to induce colitis-associated cancer. Human colonic tumors from 21 UC patients who underwent surgical resection for CAC were also studied and analyzed.
Our results show that appendectomy significantly reduced the severity of colitis and increased the number of CAC, intratumoral CD3+ and CD8+ T-cell densities were lower. Appendicitis without appendectomy led to opposite results with fewer tumors, and more CD3+ and CD8+ T cells.
We blocked lymphocyte trafficking to the colon with the anti-integrin antibody α4β7 or a sphingosine-1-phosphate receptor agonist, abolishing the inducing effect of appendectomy on tumor number and intratumoral CD3+/CD8+ density.
We also isolated CD8+ or CD3+ T cells from inflammatory neo-appendices and injected them intravenously into AOM/DSS-treated recipient mice, increasing CD3+/CD8+ T cell infiltration and decreasing tumor numbers.
In UC patients with a history of appendectomy, intratumoral CD3+ and CD8+ T-cell densities were decreased compared with UC patients without a history of appendectomy.
We conclude that, in UC, appendectomy could remove a major T-cell priming site, resulting in less effective CAC immunosurveillance.